EMS Naloxone Leave-Behind
Jump to: Resources for EMS Clinicians, Studies and Best Practices
What is EMS Naloxone
Leave-Behind?
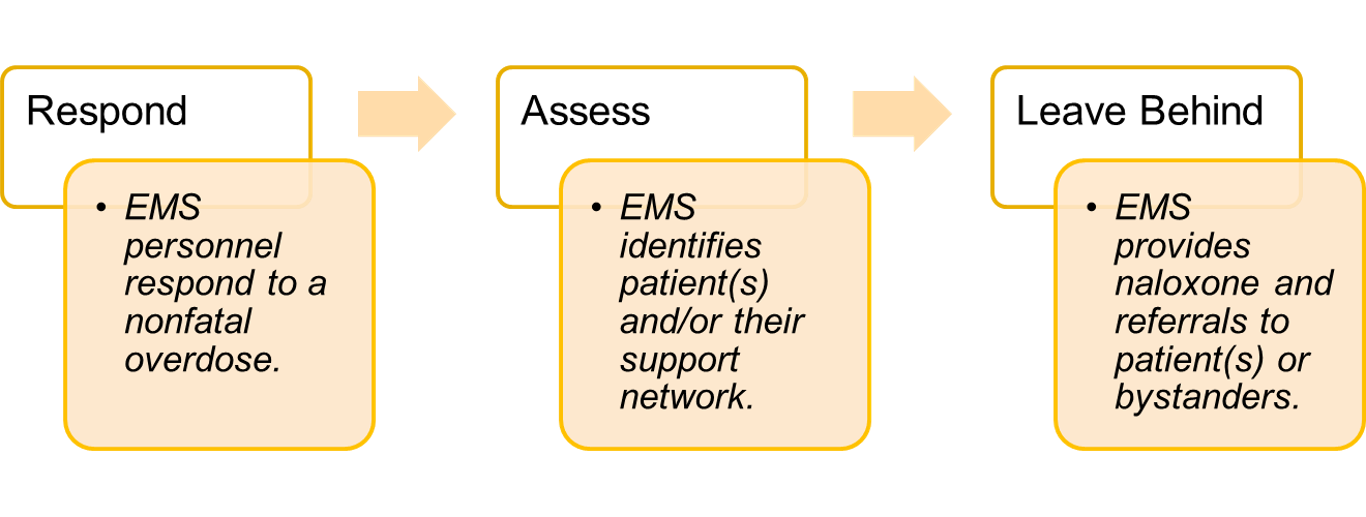
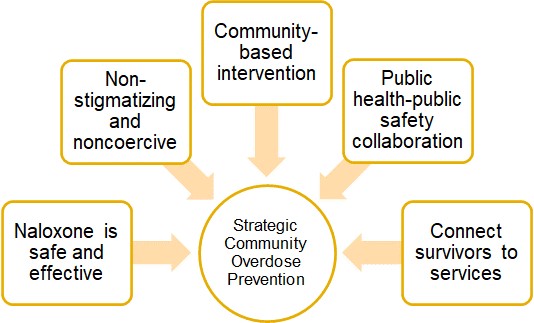
Naloxone leave-behind is a collaboration between public health and public safety that allows EMS clinicians to leave naloxone on-scene with patients and their support system.
Research shows overdose survivors face a significantly increased risk of fatally overdosing in the future. EMS personnel can help reduce the risk of fatal overdose by giving naloxone kits directly to at-risk patients and their family, friends, and roommates.
Why do Naloxone Leave-Behind?
Naloxone Leave-Behind programs improve linkages to care in the community, which can reduce future overdoses and the strain on the EMS workforce.
Naloxone is provided at no cost to EMS companies by the state of Maryland. While naloxone is not the sole answer to the overdose crisis, it can help patients live another day, improve community health, and prevent overburdening healthcare systems.
Naloxone leave-behind allows EMS professionals to directly give naloxone to exactly the people who need it the most. By providing these kits, EMS can save lives beyond the patient care given in the moment of an overdose.
Benefits of Leave-Behind
Leave-behind allows clinicians to provide life-saving resources whether a patient accepts transport or not. In the long term, connecting patients to resources can make your job as an EMS clinician easier.
First responders are uniquely positioned to interrupt the cycle of nonfatal-to-fatal opioid overdose by increasing distribution of overdose prevention resources to patients in real time.
Leave-behind kits can also connect patients to
200+ organizations that can dispense naloxone refills in every Maryland county.
Leave-Behind in Maryland
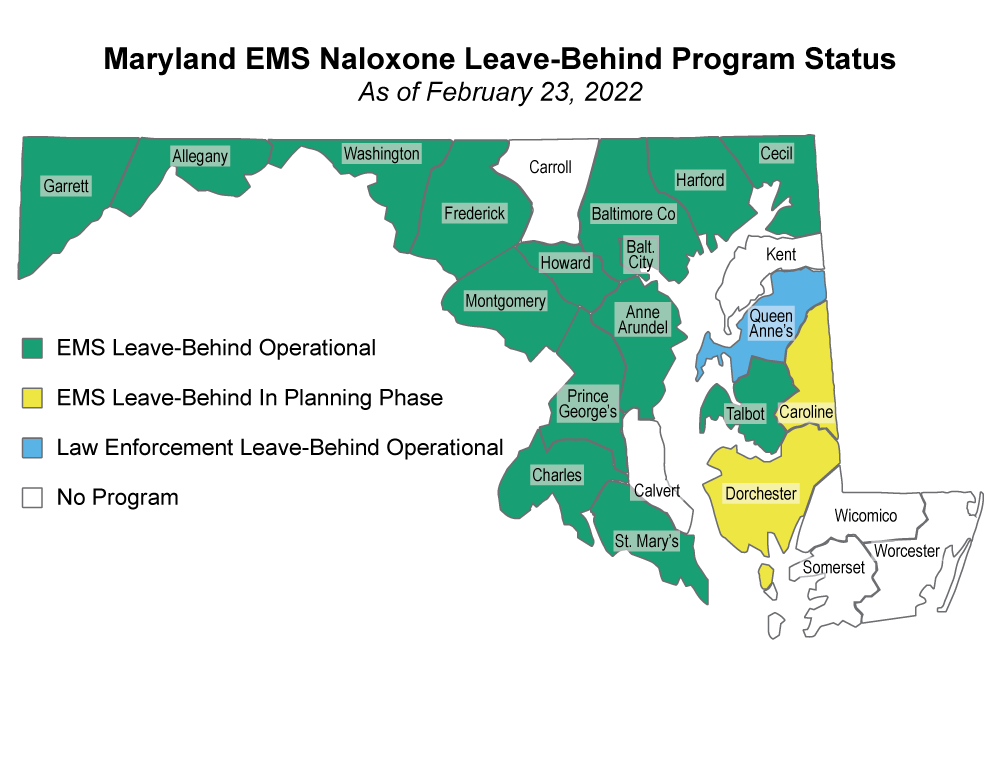
Maryland’s leave-behind program, active since 2018, is here to stay. The program is opt-in by county.
Between 2018 and 2021, thirteen jurisdictions operating EMS leave-behind programs successfully distributed 7,844 doses of naloxone to approximately 2,899 Marylanders.*
Although data is still developing on recently implemented programs in Maryland, leave-behind programs have proven successful across multiple states.
*Data as of 2/8/2022 as reported to the Maryland Department of Health Center for Harm Reduction Services through the Overdose Response Program Training Report Form.
EMS Clinicians
Video: Jason Patton on Post-Overdose Outreach
This 3-minute video explains the unique ability first responders have to intervene post-overdose, and why hope is never out of reach. Learn more at Post-Overdose Outreach.

